Canada has failed to deliver on its COVID-19 promises to the world — and some say they won’t forget it
You are reading Part 3 of Fighting for a ShotSoweto, SOUTH AFRICA — Tebogo Siwela is frank about why he signed up to have an untested vaccine injected into his arm.Mostly, for the money.When COVID-19 hit, Siwela, a lanky young musician fond of immaculately pressed shirts and trendy wide brimmed hats, was making a living showing tourists around Johannesburg, South Africa. Then, very quickly, he wasn’t.“I won’t lie. With the vaccine trial, I heard my friends talking that there’s money being offered,” he says.Vaccine trials have run at dozens of sites around the world operated under strict ethical guidelines, and organizers were typically not allowed to pay volunteers. But organizers were able to compensate participants for their food and travel. For Siwela, the baby of his family who helps support his parents, the 300 rand per visit — roughly $25 Cdn — became a lifeline.“At first I was scared, because I also thought of the long-term effects or any effects,” Siwela says of the trial. “But at the end of the day, I was like, ‘I need that money.’”Siwela lives in Soweto, a historically Black township that landed on the world’s radar in 1976 when police opened fire on schoolchildren protesting a discriminatory Afrikaans-only curriculum. As he tells his story, he’s sitting on a park bench a short walk across a public square from the spot where Hector Pieterson, an 11-year-old schoolboy, was shot and killed that day. Photographs of the boy’s limp body, draped over the arms of a fellow student, were seen around the world and helped fuel global fury over apartheid.Not quite a half-century later, Siwela explains that Soweto was hit hard by COVID-19 restrictions, and that many of his out-of-work friends joined the vaccine trial. But every time he went for a checkup or a shot, researchers would explain a bit of the science behind the vaccines, and he gradually came to believe not only in the safety of the shots, but in the importance of helping vet them for the world.Siwela’s experience is, in many ways, an illustration of how murky vaccine equity can be. The head of this particular study had pushed hard for trials to be done in South Africa, in the hopes it would help generate local effectiveness data — something that can help a local regulator make a faster decision to authorize a drug.But Silwela would go on to watch as his neighbours were left waiting for vaccines, even as they were given out to protect others around the world. Vaccine supply was initially slow in South Africa, and while the country has started to catch up, the same is not true in the rest of the African continent.In Canada, about 85 per cent of people are fully vaccinated. Only about one in 10 Africans can say the same.“Vaccine was tested here in South Africa, but being sold to other countries,” Siwela says. “That’s the saddest part. ... That’s why people feel like we were used.”The largest vaccine rollout in human history began on a hopeful note, with the global community pledging to work together to develop and share an eventual life-saving drug. That hope was snuffed out quickly.An initially limited vaccine supply triggered a frenzy in which doses were sold to the highest bidder, allowing wealthy countries to hoard the majority. The inability to pull together in a time of crisis was seen as a serious failure of multilateralism — that glue that allows different governments to work together.Meanwhile, Canada has been thrust into the spotlight, with critics pointing out that our relatively small country bought up more doses per person than any other nation on the planet. A strategy designed to ensure Canadians had early access has prompted questions about why this country — which has now administered more third doses to its own population than it has donated to the rest of the world — isn’t doing more.“We haven’t discovered any new problems,” says Dr. Madhukar Pai, the Canada Research Chair in epidemiology and global health at McGill University.“The economic inequities and the power imbalance between rich and other nations is so stuck. We say all the nice things about global solidarity, that we are all in this together, but all that it is just B.S.”The stark inequality of the rollout is teasing at the threads that normally knit the global community together, threatening to create new relationships, while fraying others.It remains to be seen whether some of the inequality will ease as vaccine production increases and demand in wealthy country wanes. But the larger question may be whether the global community will finally come back together, or further unravel.If you were new to the planet Earth, or had just not been paying much attention, the arrival of a novel coronavirus in late 2019 might require some scene-setting.The virus landed in a world already in turmoil. For the first time in decades, the global community was without the leadership traditionally provided by the United States, after years of a Trump administration that had eschewed many of t


You are reading Part 3 of Fighting for a Shot
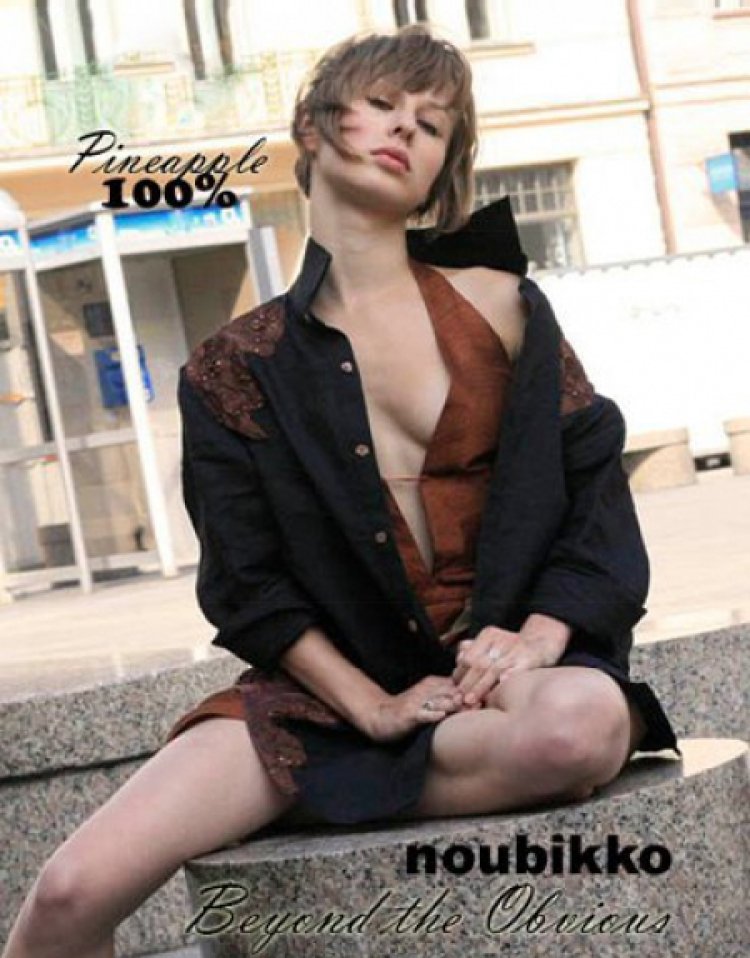
Soweto, SOUTH AFRICA — Tebogo Siwela is frank about why he signed up to have an untested vaccine injected into his arm.
Mostly, for the money.
When COVID-19 hit, Siwela, a lanky young musician fond of immaculately pressed shirts and trendy wide brimmed hats, was making a living showing tourists around Johannesburg, South Africa. Then, very quickly, he wasn’t.
“I won’t lie. With the vaccine trial, I heard my friends talking that there’s money being offered,” he says.
Vaccine trials have run at dozens of sites around the world operated under strict ethical guidelines, and organizers were typically not allowed to pay volunteers. But organizers were able to compensate participants for their food and travel. For Siwela, the baby of his family who helps support his parents, the 300 rand per visit — roughly $25 Cdn — became a lifeline.
“At first I was scared, because I also thought of the long-term effects or any effects,” Siwela says of the trial. “But at the end of the day, I was like, ‘I need that money.’”
Siwela lives in Soweto, a historically Black township that landed on the world’s radar in 1976 when police opened fire on schoolchildren protesting a discriminatory Afrikaans-only curriculum. As he tells his story, he’s sitting on a park bench a short walk across a public square from the spot where Hector Pieterson, an 11-year-old schoolboy, was shot and killed that day. Photographs of the boy’s limp body, draped over the arms of a fellow student, were seen around the world and helped fuel global fury over apartheid.
Not quite a half-century later, Siwela explains that Soweto was hit hard by COVID-19 restrictions, and that many of his out-of-work friends joined the vaccine trial. But every time he went for a checkup or a shot, researchers would explain a bit of the science behind the vaccines, and he gradually came to believe not only in the safety of the shots, but in the importance of helping vet them for the world.
Siwela’s experience is, in many ways, an illustration of how murky vaccine equity can be. The head of this particular study had pushed hard for trials to be done in South Africa, in the hopes it would help generate local effectiveness data — something that can help a local regulator make a faster decision to authorize a drug.
But Silwela would go on to watch as his neighbours were left waiting for vaccines, even as they were given out to protect others around the world. Vaccine supply was initially slow in South Africa, and while the country has started to catch up, the same is not true in the rest of the African continent.
In Canada, about 85 per cent of people are fully vaccinated. Only about one in 10 Africans can say the same.
“Vaccine was tested here in South Africa, but being sold to other countries,” Siwela says.
“That’s the saddest part. ... That’s why people feel like we were used.”
The largest vaccine rollout in human history began on a hopeful note, with the global community pledging to work together to develop and share an eventual life-saving drug. That hope was snuffed out quickly.
An initially limited vaccine supply triggered a frenzy in which doses were sold to the highest bidder, allowing wealthy countries to hoard the majority. The inability to pull together in a time of crisis was seen as a serious failure of multilateralism — that glue that allows different governments to work together.
Meanwhile, Canada has been thrust into the spotlight, with critics pointing out that our relatively small country bought up more doses per person than any other nation on the planet. A strategy designed to ensure Canadians had early access has prompted questions about why this country — which has now administered more third doses to its own population than it has donated to the rest of the world — isn’t doing more.
“We haven’t discovered any new problems,” says Dr. Madhukar Pai, the Canada Research Chair in epidemiology and global health at McGill University.
“The economic inequities and the power imbalance between rich and other nations is so stuck. We say all the nice things about global solidarity, that we are all in this together, but all that it is just B.S.”
The stark inequality of the rollout is teasing at the threads that normally knit the global community together, threatening to create new relationships, while fraying others.
It remains to be seen whether some of the inequality will ease as vaccine production increases and demand in wealthy country wanes. But the larger question may be whether the global community will finally come back together, or further unravel.
If you were new to the planet Earth, or had just not been paying much attention, the arrival of a novel coronavirus in late 2019 might require some scene-setting.
The virus landed in a world already in turmoil. For the first time in decades, the global community was without the leadership traditionally provided by the United States, after years of a Trump administration that had eschewed many of the country’s traditional allegiances.
Its one-time colonial ruler, the United Kingdom, meanwhile, was preoccupied with fallout of its own, after withdrawing from the European Union.
Populist leaders were popping up in South America, Africa and eastern Europe — many of them in countries that had traditionally been leaders in global health.
The previous decade had seen democracy on the decline and authoritarianism on the rise, says David Fidler, a senior fellow for global health and cybersecurity at the American Council on Foreign Relations. As the United States stepped back from the world stage, China and Russia stepped forward, bringing old geopolitical tensions back with a vengeance.
Even Canada, a country that had traditionally “stood shoulder to shoulder” with the U.S. on international health initiatives, didn’t really step forward, as if its confidence had been shaken by the pandemic, Fidler says.
Even though the situation ostensibly had nothing to do with global health, it meant that many of the world’s key players were too distracted by their own internal politics — or newfound struggles with other powers — to be bothered about the needs of the world, observers say.
“I’ve been involved in global health for the 25 plus years, and there are just times in the past few years where I just literally sit and hold my head in my hands, because it’s all falling apart,” Fidler says.
“Everything’s blown up.”
Like money flung into a crowd, the scarcity of vaccine supply pushed some countries to take all they could, a few to help others, and some to rail against the system.
Most people understand why countries prioritized their own populations. But there is a concept in ethics known as enlightened self-interest, which holds that if a person works to help their community, they will, in a roundabout way, end up helping themselves. It’s a philosophy meant to bind the needs of the individual to the demands of the group. A rising tide lifts all boats.
That’s where critics say the global community went awry. Countries put their own needs first to the point that the virus was allowed to circulate freely in much of the unvaccinated globe, putting everyone, the world over, at risk of a new, deadlier variant — a crushing wave that would sink all boats.
The idea of using vaccines as a political tool is not new. After crowning himself emperor, but before being exiled on an island for the first time, Napoleon Bonaparte had a son he styled the King of Rome.
In 1811, when the child was two months old, Bonaparte, very publicly, had him vaccinated against smallpox.
History may remember him as a brilliant military strategist, a revolutionary and shorter than he actually was, but Bonaparte was also an early and eager advocate for vaccination, the ripple effects of which would extend far beyond his family.
Although the first successful vaccination had happened in Paris only a decade earlier, several million French citizens had been vaccinated by 1815, thanks to a widespread government program enthusiastically supported by Bonaparte. In fact, the vaccination effort was so successful that the empire started shipping vaccine to the annexed states in Italy and the Netherlands.
For almost as long as there has been vaccine, countries have given it to their friends, denied it to their enemies, or otherwise used it as a tool of soft diplomacy.
Two hundred years later, many of the vaccine vials shipping out in recent months have arrived with invisible hopes and expectations — and that’s not necessarily a bad thing, experts point out.
“I think we should recognize that it’s not bad to act in self-interest,” says Dr. Krishna Udayakumar, the director of the Global Health Innovation Center at Duke University in North Carolina.
“In fact, from a global health lens, I think we have done ourselves a disservice by focusing perhaps too much on the humanitarian lens and not enough on the self-interest.
“We know that vaccinating the world and leading an effective global response is important for moral and ethical reasons. It’s important for equity. But it’s also important for self-interest, including the national security, health and economic recovery of populations in high-income countries.”
China is widely regarded as having used vaccines to burnish its international reputation, arguably part of its Belt and Road Initiative, meant to use investment to curry influence around the world. As Omicron loomed last fall, China committed an additional 600 million doses to relatively unprotected Africa.
Russia’s homegrown dose, named Sputnik V in a clear reference to the world’s first satellite and the power and prestige Russia wielded during the space race, has sent doses around the world. It’s also ruffled feathers in Europe, where eastern European countries such as Hungary bought up large quantities of the shot while waiting for the European Union’s distribution to scale up.
A Russian invasion of Ukraine is feared to be imminent, and in recent months Ukrainian officials had accused their powerful neighbour of pushing anti-vaccine disinformation in a bid to undermine sovereignty, including, according to the Washington Post, conspiracy theories that the virus was spread via 5G networks of by Bill Gates. (The Kremlin has denied doing this.)
With a vaccination rate that has lagged behind much of the continent, some reports have suggested that Ukrainians in traditionally pro-Russian areas have remained unvaccinated because they wanted a Russian vaccine, and weren’t able to get one.
The dreams of the two would-be vaccine powers didn’t totally come to fruition, Udayakumar says. China’s vaccines haven’t been as effective against Omicron, which has dampened the appetite for them abroad, while Russia has had issues scaling up production, he says.
Meanwhile, low-income Cuba made its own vaccine — two, in fact, so far — and has started looking at donating to other poor nations. In interviews, the makers of the vaccine have credited decades of embargoes imposed on the Communist nation for granting them an independent streak that pushed them to create a homegrown dose. (It doesn’t hurt, either, that the country has a well-oiled biotech sector thanks to Fidel Castro, who pumped at least a billion dollars into the industry.)
According to a peer-reviewed medical journal called the BMJ, Cuba already exports hundreds of millions of vaccine doses, including the world’s first meningitis B vaccine, to more than 40 countries. Perhaps unsurprisingly, it’s been in talks with other countries about possible deals for its COVID vaccines since last year. Cuba now has two vaccines in circulation, Abdala and Soberana, named, respectively, for a poem written by a hero of independence and the Spanish word for “sovereign.”
The prospect of selling shots abroad could become a badly needed economic boost for a country where the pandemic has emptied some store shelves and sent inflation soaring.
When India, one of the world’s vaccine-making powerhouses, was hit by a devastating COVID wave in the spring of 2021 it cut off exports of shots to the rest of the world, putting a major kink in the world’s supplies. The global scheme to share vaccines, known as COVAX, was particularly hard hit. The shortfall played a role — in addition to donation shortfalls from wealthy countries and general manufacturing backlogs — in the scheme missing its goal to deliver two billion doses in 2021 by roughly half. In early 2022, Seth Berkley, the head of GAVI, the global health organization that co-founded COVAX, said they were “basically out of money” as the program launched a fundraising bid for an addition $5 billion to continue its work.
Meanwhile, South Africa, a country seething for having been blamed for detecting new variants and notifying the world, is looking to take back a piece of global vaccine production. The move is arguably part of a larger push for African solidarity, as the continent has slowly been left behind by the wealthy world. As COVAX stumbled, the African Union assembled a task force, called the COVID-19 African Vaccine Acquisition Task Team, or AVATT, to start buying shots just for the continent.
Until recently, the United States has been noticeably absent from the global conversation, as President Joe Biden has struggled to get a global vaccine program up and running, but is looking to scale up this year.
The U.S. has now shipped roughly 400 million doses to other countries, which is more than all other donors combined, but is still far less than what they’ve pledged.
“We’re unfortunately stuck in the game of saying who’s doing more as opposed to reflecting whether we’re doing enough,” Udayakumar says.
As the tectonic plates of global politics shift, Canada’s reputation is in flux.
While federal politicians here have stressed the need to vaccinate the world, critics have slammed the fact that while millions of vaccines have been pledged, only a fraction have been delivered.
The federal government has purchased more doses per person than any other country, and in recent months has pledged to direct some of that largesse to countries without the pockets to fund vaccine contracts. But of the 50 million doses so far, Canada has delivered just 12.7 million. Of the 150 million doses it has promised to buy COVAX? Only enough cash for 84 million doses — roughly $545 million — has been contributed.
International Development Minister Harjit Sajjan stresses that Canada is moving as quickly as possible on donations, and that it’s equally important to make sure that recipient countries are prepared to accept the vaccines they receive: “I’ve seen the impacts of crisis like this, that it has on poor developing nations,” he told the Star.
Sajjan, who did three tours in Afghanistan as a military reserve officer, says those nations need appropriate support to distribute vaccines.
“The key word being ‘appropriate’ support,” he says. “How are we taking the viewpoints of the population itself? That’s very important. It’s one of the biggest lessons I’ve learned being on the ground in crisis areas.”
Nonetheless, since early December, when the federal advisory panel recommended everyone over 50 get a booster dose, more than a million shots has arrived on Canadian soil every week.
There are those that fear Canada’s reputation is taking a black eye that won’t be healing anytime soon — and will have effects beyond COVID.
“Canada will not be remembered as an ally in the fight against COVID,” says Fatima Hassan, a South African lawyer who has been one of the loudest voices for global vaccine equity.
“It’s on the wrong side of history, and, you know, there are places in South America and Africa that will never forget this. You could have done something to help and you chose not to.”
When it comes to the current Canadian government, Lauren Dobson-Hughes, a consultant specializing in gender, health and rights who has done some work with COVAX, argues that development has never been a major focus.
“Politically, development issues are not the priority for them, they have never been won over by it, it does not excite them, they don’t get it, which is a shame, because we see how critical global development is to Canada’s and to our collective well-being,” she says.
She argues that translated into political polarization when early polling showed that almost three quarters of Canadians didn’t want to see doses sent to other countries before everyone in the country had been fully vaccinated. (According to newer numbers from Angus Reid, there’s been a significant shift in public perception since, with almost half of the population now favouring sending doses overseas.)
“It strikes me that both for vaccine equity and getting the world out of this trend at the moment, of authoritarianism and individualism, some sort of shift back to mutuality and common humanity is needed.”
Sitting in her office, a bright white box in a tower overlooking the Angolan coastline, flooded with sunlight, Dr. Djamila Khady Cabral recalls the optimism she felt when the first vaccines began to move around the globe.
“I didn’t believe that we would arrive at this situation,” she says, sounding slightly incredulous. “I would say, ‘No, no, no. They will find a way. They will give some to COVAX.”
But the reality of what actually happened has been a bewildering experience for Cabral, a public health expert who has worked across Africa for the World Health Organization. Now the organization’s representative in Angola, West Africa, she’s seen first hand how the lower-income country has worked mightily to be ready for COVID vaccines, only to be left waiting as shots increasingly flowed to wealthier nations.
“How is it possible for a country that has many vaccine doses available for every person — even children — knowing that other countries are running out of it? Do they have not have this sense of injustice?”
In December 2021, the members of the World Health Organization agreed to come together and create a new pandemic convention or agreement, in the hopes of hammering out a better way of preparing for pandemics and hopefully avoiding some of the mistakes made during COVID-19.
The decision was “historic,” according to Dr. Tedros Adhanom Ghebreyesus, the WHO director-general.
“The COVID-19 pandemic has shone a light on the many flaws in the global system to protect people from pandemics: The most vulnerable people going without vaccines; health workers without needed equipment to perform their life-saving work; and ‘me-first’ approaches that stymie the global solidarity needed to deal with a global threat,” he said at the time.
Fidler, from the Council on Foreign Relations, has his doubts about the value of a treaty — which he says most countries wouldn’t stick to anyway.
Instead, he argues that some of the geopolitical battles will have to be dealt with first, whether that means the U.S. and China sorting out some of their issues, or that low-income countries will have to get in on the act, like during the Cold War, when he says some became good at playing the United States and the Soviet Union off each other.
He worries that the pandemic has only weakened the forces that connected the global health community, and that if countries fail to band together here, they will fail again when the next pandemic comes, or to ever work together on meaningful action on climate change.
Having a potential legal instrument that would speed up things such as information sharing in a crisis, or perhaps even include rules on access to medicine, could “potentially be transformative,” according to Roojin Habibi, a lawyer specializing in global health law.
Though at this point, discussions are only beginning and it’s not clear what the future will hold. But if there’s one word that she could bar from use when talking about the pandemic, it’s “unprecedented.”
Habibi, also a research fellow at the Global Strategy Lab at York University, points out the world has weathered storms of disease and inequality before — notably, HIV. Even then, life saving drugs trickled out to the developing world long after they’d become available in wealthier nations, and only in response to advocacy. Even now, many of the fault lines seen in the global rollout trace old colonial or socioeconomic divides.
The problem, she argues, with talking about the pandemic without couching it in the history that came before is it creates a sort of political tabula rasa, where leaders are forgiven for not doing what they know needs to be done.
“My fear with using the word ‘unprecedented’ all the time is a word excusing ... leaders from taking action.”
In Angola, being the official face of Canada has traditionally meant a lot of paperwork.
For decades, the country’s honorary counsel — a volunteer position that mostly involves helping the country’s roughly 900 Canadians access services and find information and sort out the forms that accumulate when living abroad — has been a tall, kindly architect named Allan Cain.
Cain moved to the country in the 1970s, intrigued by a newly independent government interested in revamping its urban design. While the country plunged back into war, he ended up staying and running an NGO that, among other things, tries to improve conditions in slum areas.
But more recently, his duties have included being on hand for a shipment of COVID vaccine donated by Canada that arrived in the sprawling east African country, and speaking to local reporters about why the snowy, faraway country had shared them.
Afterwards, over burgers at a beachside restaurant in the capital city of Luanda, he describes the way in which the country he now calls home has struggled mightily to heal from decades of war.
Canada has traditionally been seen here as an ally in that fight, dating back to the schools run by Canadian missionaries in the 1800s. Much of Angola’s eventual independence movement would grow out of those church schools.
A doctor originally from Ontario, Dr. Walter Strangway, is also remembered fondly for the 40 years he spent working in the country, starting in the late 1920s. During his time in Angola, he performed a reported 40,000 surgeries and was renowned for his work with people with leprosy. (A new 250-bed hospital named for him was opened in 2020.)
Even now, Cain says, the Canadian government was one of the first to help fund projects to help mitigate the spread of COVID here, including his NGO’s work to improve water access in slum areas.
It’s this legacy of support that drew him to the consul job, he says. “That’s why I’m happy to represent Canada here,” he says. “I do it as a volunteer.”
“Years ago, there was a slogan promoted by the Canadian consular service. It was a bit corny, but it was ‘The caring face of Canada,’” Cain says. “And I think that’s the image that certainly we have in Angola.”
But it’s a reputation he worries might be at risk, beginning with Canada withdrawing from the Kyoto protocol — an international agreement on carbon emissions in 2011. He notes that Canada has lost recent bids for a security council seat. As climate change escalates, he worries about Canada not having a say and a role to play in global conversations.
“I think in the long term, Canada’s role in climate-change issues is going to be probably more important than the short-term COVID (response).”
One of the many reasons vaccines can take longer to get to low-income countries is there is a lack of data on how they work in those countries, so even before the first COVID vaccine candidates began go show glimmers of hope, Shabir Madhi jumped into action.
Madhi, one of the South Africa’s most high-profile vaccine experts, wanted there to be South African data, in the hopes that it would speed the process of getting an eventual vaccine into the country.
“I really had to make a case to Novavax to actually do the study in South Africa, so it’s been weeks, months, convincing them that that was what they needed to do.”
Pharmaceutical companies often don’t test in the Global South, and many of the regulators in northern countries would insist on data from their own populations before green-lighting a vaccine.
In some ways, Madhi’s efforts worked, in that South Africa got COVID vaccines months after wealthier countries, instead of years.
Yet, Madhi questions whether anything will actually change in the long term, as long as northern countries and pharmaceutical companies continue to prioritize themselves, as long as research institutes use Africa as a training ground, he argues, and not much more.
“You can only bring about a fundamental change when you are equal partners in a relationship,” he says.
“If you’re always the orphan in the relationship, the chances of being able to make any sort of substantial movement in relationships doesn’t exist in anyone’s mind.”
The unequal way vaccines were created and rolled out won’t be soon forgotten.
Alex Boyd is a Calgary-based reporter for the Star. Follow her on Twitter: @alex_n_boyd